What Climbers Should Know About Lumbricals (Pain After Climbing Pockets)
Hooper’s Beta Ep. 83
INTRO
As climbing has progressed in popularity and difficulty, climbers have been able to pull off incredible new moves that were once considered impossible. This inevitably means our bodies, and especially our fingers, are being pushed to new limits. But pushing the boundaries doesn’t come without a price. And lately, one of those prices has been the rise of an injury to a rather odd and even mysterious muscle.
VIDEO OVERVIEW
These injuries are typically due to pockets, or just hitting small holds with just 2-3 fingers, causing some fingers to remain in the extended position while an adjacent finger or two goes into a flexed position.
In this episode, we’re taking an in-depth look at these weird muscles in our hands called Lumbricals. We’ll talk about the structure of lumbricals so you can understand why they’re important and how they get injured, and we’ll go over how to test for a lumbrical injury as well as some general rehab advice. We’ll also have a separate video with detailed, step by step instructions on how to recover from a lumbrical injury, so keep an eye out for that.
Let’s get started with a little anatomy review of the lumbricals and what makes them so special.
PART 1: ANATOMY OF THE LUMBRICALS
The lumbricals are quite unique for a variety of reasons. For one, they originate AND insert in the hand, making them an intrinsic muscle. This is in contrast to an extrinsic muscle like the flexor digitorum profundus, which begins at the elbow and ends in the fingers!
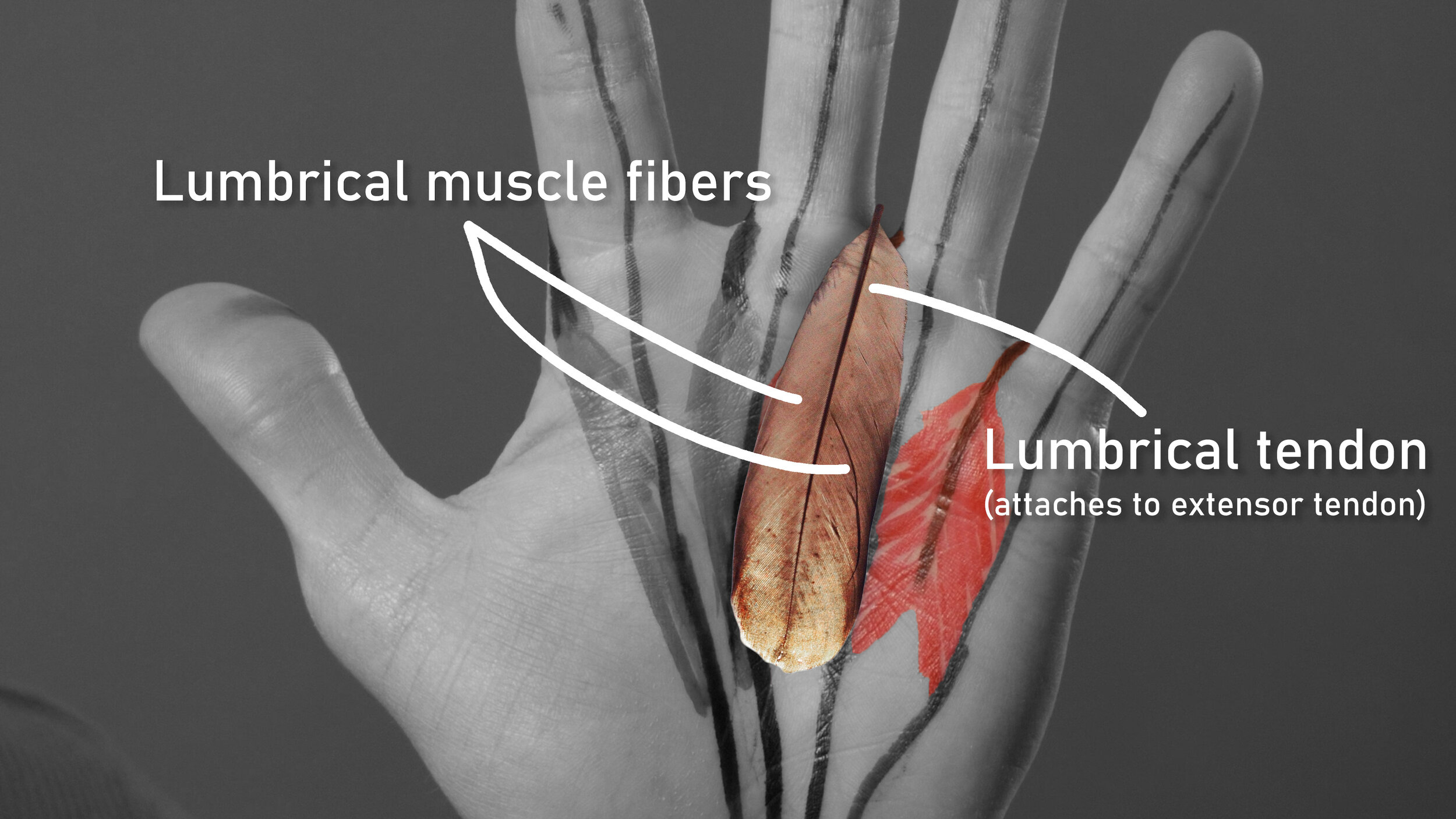
Secondly, they’re not attached to any bones! They’re actually only attached to tendons, specifically the flexor digitorum profundus in the palm and extensor tendons in the fingers, which means their attachment points are completely mobile; they change position as the FDP and extensors move.
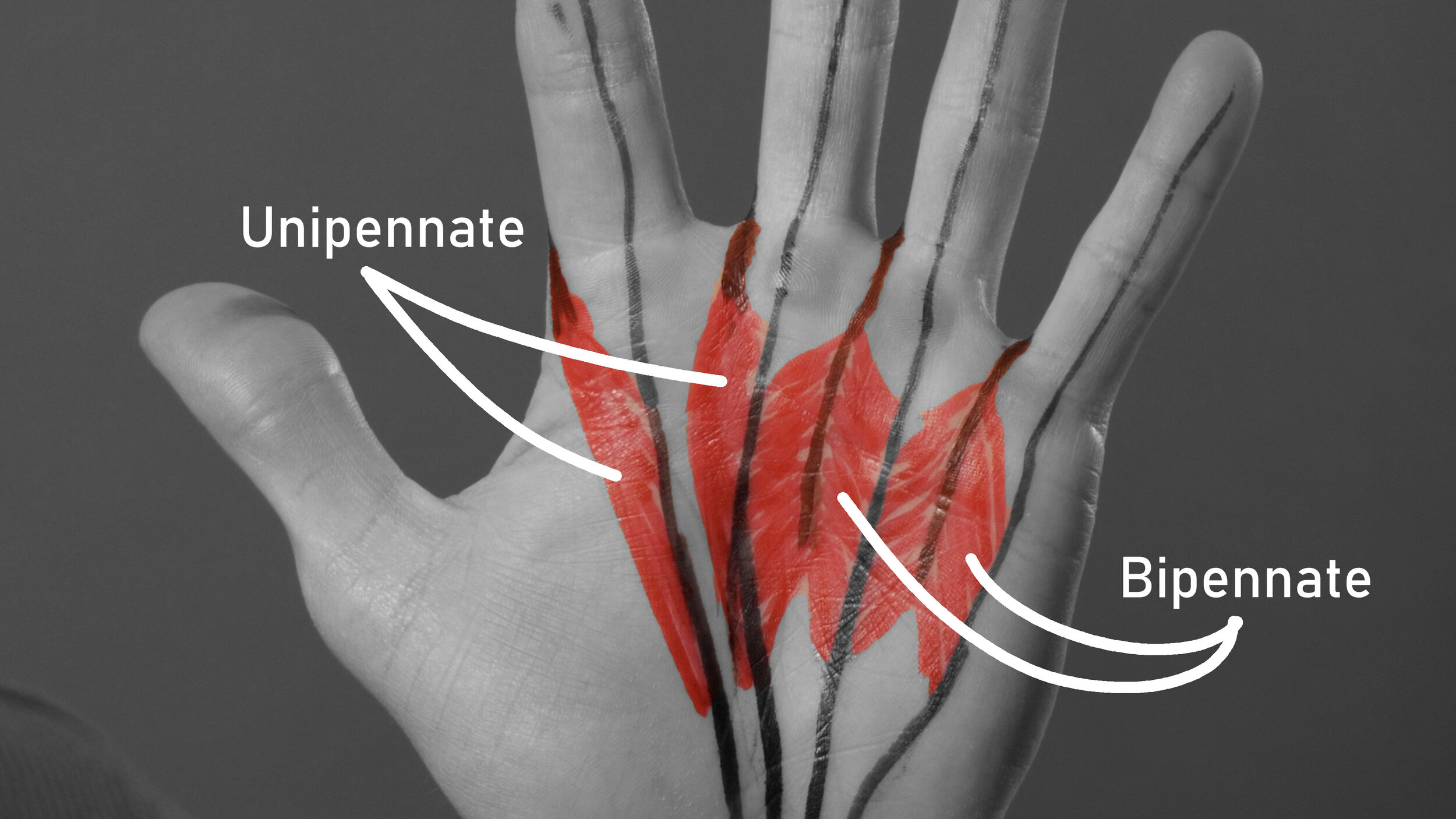
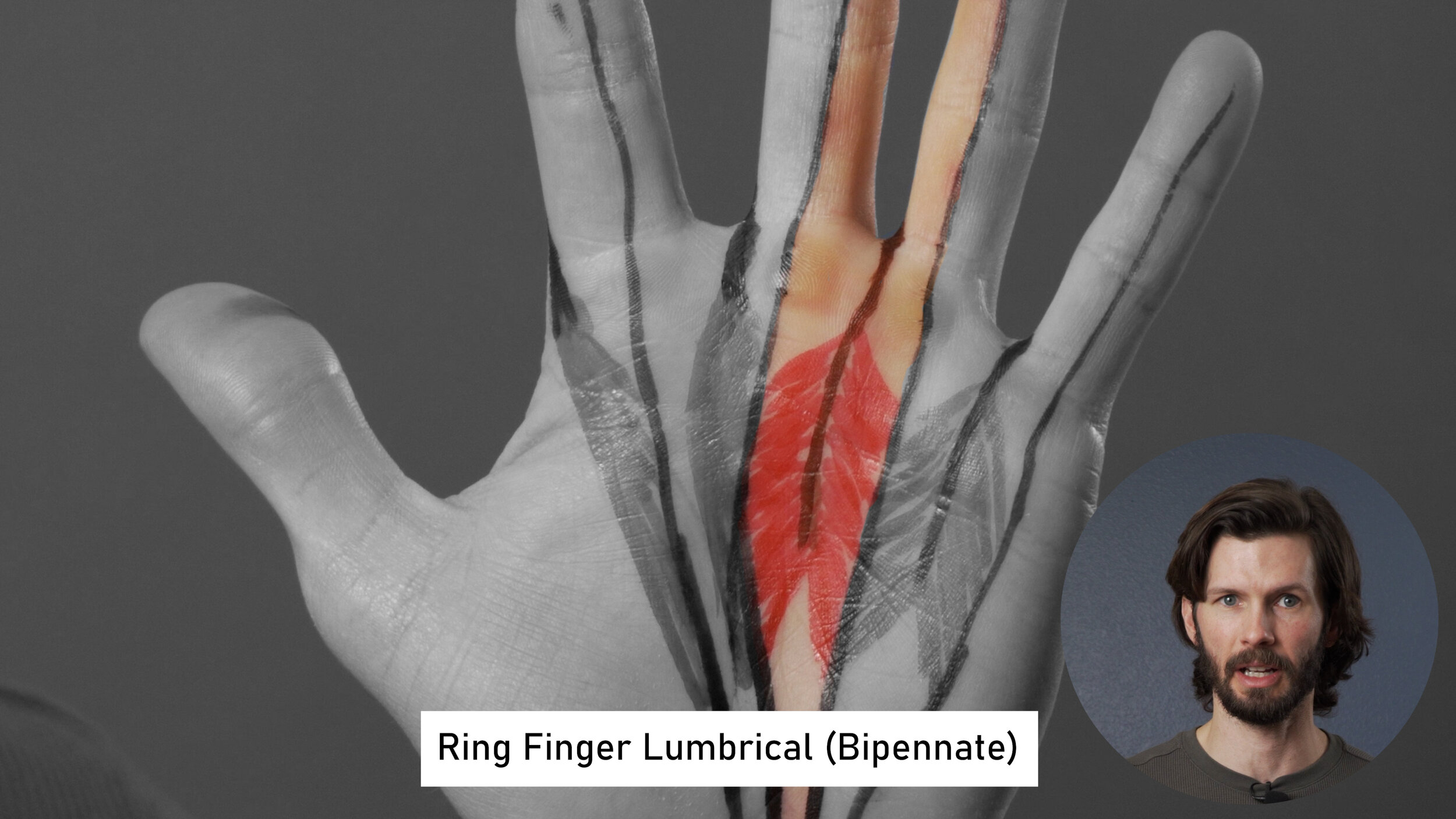
Thirdly, and most important for understanding how they get injured, the lumbricals of the pinky and ring fingers have a bipennate structure, while the middle and index fingers are unipennate.
A bipennate muscle is like a feather. The barbs of a feather go in opposite directions on either side of a central quill. With a bipennate muscle, the “quill” is a tendon and the “barbs” are muscle fibers. The muscle fibers of a bipennate lumbrical attach to the extensor tendon (the “quill”) of one finger and the flexor tendons of two fingers. This can lead to problems if those two fingers are moved in opposite directions while under force.
So the pinky finger has half the lumbrical muscle fibers from the side of the pinky and the other half from the ring finger. The ring finger has half on the ring finger side and half the middle finger. The middle and index, though, are unipennate in structure, meaning that the muscle fibers are all oriented in one direction as they each originate at one tendon.

PART 2: ROLE OF THE LUMBRICALS IN CLIMBING
The mobile attachment sites of the lumbricals made it hard to study their actual function, but researchers eventually settled on one main conclusion: the lumbricals primarily act in a sensory role, helping maintain a healthy balance between the finger flexors and extensors. More specifically, the lumbricals provide feedback on the force generated at the flexor digitorum profundus and the extensor tendons to make sure one doesn’t overpower the other and create an issue or injury.
What does this mean for climbers? Well, first, with anything in our bodies, there needs to be balance between the various parts for it to function healthily and get us up the rock. Since climbing relies heavily on the finger flexors compared to the extensors, we need the lumbricals to make sure those tendons don’t become too imbalanced as that could lead to malfunction. In other words, if the lumbricals sense a large discrepancy between the force created by the flexors versus the extensors, the body will limit the amount of force produced by the flexors to help bring things back into balance and prevent an injury.
Additionally, there is evidence to show that the lumbricals provide information regarding the position of the DIP and PIP joint, particularly while the MCP joint is slightly flexed. This position is also where the lumbricals are most active in a mechanical role (rather than just sensory one), meaning they also add some, albeit small, mechanical stability to the joint. Therefore, we can conclude that the lumbricals are particularly important for the healthy function of our hands when on slopers and pinches.
Now you might be thinking, “Oh snap, I’m just gonna train lumbricals for a month and I’ll be climbing slopers and pinches like a BEAST!”
Not so fast! The lumbricals are actually weak AF. Research has shown they only contribute about 2% to the flexion strength of the MCP joint. Basically, the lumbricals aren’t going to directly help you grip really hard. Rather, the sensory feedback they provide allows other parts of your hand to do so without injuring themselves.
So what happens to the function of your hand if you injure your lumbricals?
Mainly, injured lumbricals will have a reduced ability to provide the needed sensory feedback in the hand, which means your body won’t be able to maintain that all-important balance as effectively. This may prompt your body to limit force production in the hand for fear of injury, meaning you won’t be able to hold on at your usual strength. Also, since their role is so sensory, lumbricals help with dexterity. Losing dexterity may have a small impact on precision movements with climbing, as well as in your everyday activities -- you know, the things you do when you don’t get to climb.
Now that we know how the lumbricals work and what their function is for climbers, let’s talk about how they get injured in the first place.
PART 3: HOW THE LUMBRICALS GET INJURED
Injuries to the pinky and ring-finger lumbricals are somewhat common due to their bipennate structure (recall the feather example). An injury happens when one finger remains extended while the adjacent finger(s) flex. As you can probably imagine, this can happen easily when climbing on pockets or if you just don’t get all of your fingers on a small hold.
Let’s use a 2 finger pocket as an example. Imagine that the ring and middle finger are in the pocket, and the index and pinky are not. Typically this means that the ring and middle will be extended with a mild amount of flexion, while the index and pinky are fully flexed and curled up into a little ball of pain.
Remember that the lumbricals attach to tendons, so in this position the extended ringer finger is pulling one side of the lumbrical in one direction, and if the adjacent finger is flexed, it is pulling in the opposite direction. Think back to our feather example. Grab your imaginary feather from either side and pull in opposite directions. You’re going to shred your feather.
Now, just flexing one or two fingers is not the issue. I mean, I can stand here and do this [mimics pocket position with hand] all day without damaging my lumbricals. The issue is applying heavy force through the finger when they’re in such differing positions. Because of this, it is actually safer for the lumbricals to try and leave as much of the finger not in the pocket extended if you can, but that’s a topic for a whole other video *wink*.
But what about the unipennate lumbricals of the index and middle fingers? These are much less likely to be injured because of that structural difference, and have been shown in studies to actually be stronger than the bipennate lumbricals.
So now we know how a lumbrical gets injured, but what does it actually feel like?
PART 4: SYMPTOMS OF A LUMBRICAL INJURY
OK, so… you did some gnarly pockets, or you hit a tiny hold and your pinky missed and you curled it all the way up for max gnar, you finished the proj, got to the top and yelled “YEW!”
But moments later your ring finger is killing you and you think you just ruined your climbing trip. How do you diagnose a lumbrical injury?
The first step is determining if you have the right symptoms. A lumbrical injury will typically present with pain in the palm of the hand, up to or near the base of a finger and perhaps into the region near the A1 and/or A2 pulley. For this reason, it is possible that it can feel like a pulley injury when it is not. The pain is typically not in the direct center of the finger (or that finger’s flexor tendons), but rather slightly on the side of the finger (or tendon) on the palm side.
Symptoms are typically more of a dull ache, but can feel like a sharp pain particularly if the lumbrical is stressed. Which brings us to the next point, the lumbrical stress test.
PART 5: LUMBRICAL INJURY TESTS
The lumbrical stress test is the main way to diagnose a lumbrical injury. To perform this test, extend the injured finger while slowly flexing the adjacent fingers. This can be done passively or actively. Actively means that you do this under your own volition. Activate the extensors on one finger while actively flexing the adjacent. Passively would mean using the other hand (or a friend, if you have one) to hold one finger in extension while flexing the others.
I recommend actively first because you will naturally start to flex the injured finger which will help protect it. If there is not a lot of pain, then try the passive test. If this passive or active motion alone causes pain, do not continue; you can safely suspect a lumbrical injury at this point.
If this first step does not cause pain, though, and you have gone through the full range of motion, perform the following: while in this position of being extended and flexed, apply gradually increasing pressure near the tip of the injured/extended finger, forcing it to engage in flexion. The injured finger should remain relatively extended while the adjacent fingers remain flexed. The degree of flexion of the adjacent fingers compared to the degree of extension of the injured finger will affect the amount of strain/stress on the lumbrical, so this is your tool to determine the severity of the injury. However, do not apply more force than is needed to produce mild, if any, pain. There is no need to suffer and make your injury worse!
Mild-moderate strain (Grade I) and no tearing: If you had to apply significant pressure, or take the finger through a large amount of flexion vs extension then you may have a simple low to moderate level strain and likely no tearing.
Moderate strain (Grade II) and/or low grade tear: If you were able to get in position without pain and were able to load the finger with mild to moderate force before eliciting pain, the injury may be more of a moderate strain or perhaps a low grade tear.
Significant Strain (Grade III) or mild/moderate tear: If you felt pain simply going into the flexed vs extended position you may have a significant strain or a mild to moderate tear.
Significant tear: if you have significant pain and loss of function, you may have a higher level injury that may need to be assessed immediately by a medical professional and you shouldn’t really be watching this video. This severity of injury is unlikely with most climbing injuries unless there was a form of trauma involved. As such, it will not be a focal point of this video.
Note: the timeline of the injury may affect the testing results. If you injured it climbing and are doing these tests 5 minutes later, you may need to retest 10, 30, and/or 60 minutes later to get a full picture of the injury. If you’re testing 1-2 weeks later, adrenaline and acute swelling may no longer be a factor and testing results should be more accurate.
PART 6: DIFFERENTIAL DIAGNOSIS
Now comes the tricky part: the potentially misleading factors to a lumbrical injury are numerous. Here are some comparisons to help you figure out if you have a lumbrical injury or something else.
Lumbrical injury vs an interpalmar plate ligament injury
Location is your best friend here. An interpalmar plate injury will be much more localized to the space between your metacarpal joint and will not likely cause pain in the palm of the hand and definitely not near the A2 pulley. Flexing one finger and extending another and loading the finger will not provide as clear-cut information with this injury, so rely more on location.
Lumbrical injury vs an interosseous muscle injury
This one isn’t too bad. There are dorsal and palmar interossei muscles in the hand.
The dorsal interossei muscles are bipennate, so they can suffer a similar fate as the lumbricals. To differentiate a lumbrical from a dorsal interossei injury follow these steps.
With your injured hand, extend all of your fingers and try to separate them from one another, essentially making your hand as wide as possible.
Next, take your uninjured hand and now lightly try and force two fingers at a time back together. Don’t push too hard because those interossei muscles are pretty weak.
Resisting this squeeze would create pain with a dorsal interosseous injury, but not likely with a lumbrical injury.
The palmar interossei are even easier to differentiate. They adduct the same digits or bring them TOWARDS the middle finger. They are also unipennate so they are not likely to suffer from a pocket injury and will not likely be positive with the flexion/extension test. To further confirm, bring the fingers together and then try to forcefully separate them. Pain with this may indicate a palmar interossei injury but would not likely cause pain with a lumbrical injury.
Lumbrical injury vs a pulley injury
This one is a little easier. The lumbrical will likely only cause discomfort when isolating the injured finger, so recreating the pull WITHOUT flexing the adjacent fingers will help here. Also, the A2 pulley injury will be more easily aggravated in the crimp position and less painful in the open hand position
Lumbrical injury vs a flexor digitorum injury
This one is also somewhat easier. A lumbrical injury will have the worst pain when the injured finger is extended and the other fingers are flexed. Once you place the adjacent fingers in extension as well, the pain should reduce or eliminate. If you have a flexor digitorum injury instead, you will likely have pain in both positions.
If you are still feeling unconfident in diagnosing this injury, please reach out to a skilled professional for further evaluation and diagnosis of your injury!
PART 7: REHAB ADVICE
Rehab for this injury can be a little tricky as there can be many factors to consider. For that reason, we’ll have an entire video dedicated just to that. BUT, here’s some general advice to help get you started, broken down into 4 components: range of motion, stretching, tissue mobility, and retraining. Don’t do any of these activities if they cause you more than a 2 or 3 of 10 on the pain scale.
Range of motion: Your best bet for an initial injury is just to perform gentle, active range of motion. This can be performed almost immediately, or within the first few days of an injury. Pick 3 rows on the palm of your hand at the base of the palm, middle of the hand, and towards the knuckles. Start with your fingers fully extended, then flex your fingers until the fingertips touch those rows. Though it may seem somewhat similar, this is not tendon gliding; it’s just range of motion. You’ll also want to focus on creating an “L” position with your hand, as this will lightly activate the lumbricals. Perform to tolerance multiple times a day.
Stretching: You’ll want to perform light stretching of the lumbricals. This will include two different stretches. One stretch will be extending at the MCP while flexing at the DIP and PIP. This will be assisted by your uninjured hand. The second stretch will be to stretch the affected finger into extension and the adjacent finger into flexion. This will create a more aggressive stretch though so be conservative here. You can start these stretches immediately, or within the first week of your injury depending on the severity.
Tissue mobility: Any type of self massage here is great to help stimulate healing. Use your hand and some lotion or a massage tool and simply stimulate the tissue for 5-10 minutes as needed. You can start this immediately with a mild injury, or once any swelling or pain decreases with a more significant injury.
Retraining: This is definitely the longest and hardest section so you’ll definitely want to check out our other video for all the details there. But a few tips for this would be working on the “iron claw” technique to get those flexors and extensors activated while moving the lumbricals. For this you would grip a dowel or highlighter between the tips of your fingers and near the base of your finger on the first phalange. Squeeze tight, keeping your DIP and PIP flexed and then attempt to extend at the MCP. You can also do strength training techniques for the lumbricals such as L pinches, farmer pinch carries, and even just general climbing! However, you’ll want to avoid climbing on pockets until your lumbricals are more healed. Retraining can begin once you can go through full range of motion, gentle stretching, and tissue mobility without significant pain.
OUTRO
Before we go, I want to leave you with one final note. The prognosis around most lumbrical injuries is good! If you work on your range of motion, tissue mobilization, stretching, and retraining, you can definitely restore function and return to climbing hard.
And that’s it! I hope you found these little muscles to be as interesting as I did. The more we know, the better we can assess ourselves, our injuries, and our climbing capabilities.
Until Next Time…
Train those brain cells to make you sound heckin cool when talking climbing with your friends. Climb those pinchy monsters and explain how the lumbricals are the true heroes in this scenario.
Send it using an unnecessary pocket just for show. …. Maybe don’t repeat those ones.
Disclaimer:
As always, exercises are to be performed assuming your own risk and should not be done if you feel you are at risk for injury. See a medical professional if you have concerns before starting new exercises.
Written and Produced by Jason Hooper (PT, DPT, OCS, SCS, CAFS) and Emile Modesitt
IG: @hoopersbetaofficial


















